The Benefits of CCM for Health Systems With all the current advancements in healthcare, Chronic Care Management (CCM) has become imperative, especially for hospitals and clinics struggling with more and more people having long-term health problems. Chronic Care Management is … Read More
Blog
The Benefits of CCM for Patients
The Benefits of CCM for Patients Chronic Care Management (CCM) and Remote Patient Monitoring (RPM) are revolutionizing the healthcare landscape, especially for those battling chronic conditions. CCM refers to a comprehensive approach to managing chronic diseases, emphasizing regular coordination and … Read More
Buzzwords in Modern Healthcare
Beyond Buzzwords: How Chronic Care Management Is Revolutionizing Patient Health Over the past decade, the healthcare industry has been inundated with exciting buzzwords promising to revolutionize the way healthcare is delivered. Words like “analytics”, “AI”, “precision medicine” and “blockchain,” have … Read More
Inauthenticity: The Downfall of Medical Innovation
Inauthenticity: The Downfall of Medical Innovation The next monumental leap forward in medical science and patient care is finally here—or so many overzealous healthcare press releases declare. While every health system hopes to enhance its services with the next generation … Read More
The Chronic Care Nurse of the Future
The Chronic Care Nurse of the Future Signallamp Health provides cutting-edge healthcare with its chronic care model of nursing. In the rapidly evolving landscape of healthcare, where patient outcomes and care quality take center stage, the need for effective chronic … Read More
What is Transition of Care?
What is Transitional Care Management and How Does it Help Patients? Transition of Care (TOC) is a CMS reimbursement intended to help patients as they move from an acute setting back to the community. A smooth transition back home is … Read More

The Many Benefits of Chronic Care Management
The Many Benefits of Chronic Care Management Chronic care management (CCM) is a healthcare approach designed to address the complex needs of patients with chronic conditions. When properly executed, a remote chronic care management program can be a win-win for … Read More
Increasing Physician Capacity With CCM
Increasing Physician Capacity With CCM In July of 2022, Justin Porter, Assistant Professor of Medicine at the University of Chicago Medicine and a team of other researchers published a study in the Journal of General Internal Medicine titled: “Revisiting the … Read More
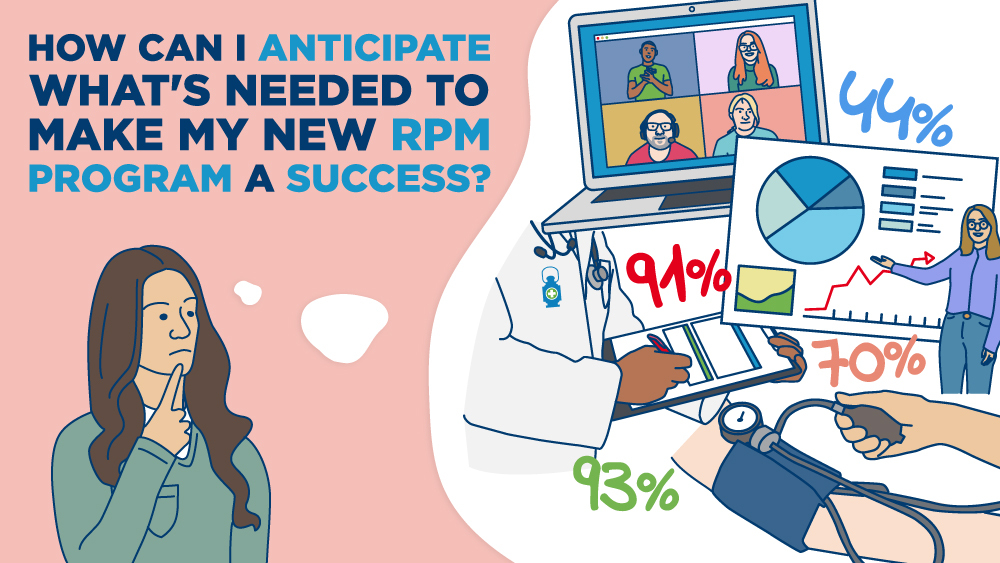
How Can I Anticipate What’s Needed to Make My New RPM Program a Success?
How Can I Anticipate What’s Needed to Make My New RPM Program a Success? Remote patient monitoring (RPM) technology is in high demand as more healthcare providers and health systems search for better and more effective ways to care for … Read More
2 Critical Resources Patients Need Upfront for An RPM Program to Succeed
2 Critical Resources Patients Need Upfront for An RPM Program to Succeed If your hospital, clinic or healthcare facility provides care to patients with chronic conditions, remote patient monitoring (RPM) can help improve your patients’ outcomes and overall engagement. The … Read More